Innovation
The budding promise of 3D biopsies
Researchers have discovered that existing optical fibre technology could be used to produce 3D images of tissue inside the body, allowing clinicians to examine living tissue in real-time. To find out more, Chloe Kent spoke to Dr Antony Orth, who has been leading the development of the technology at RMIT University in Melbourne, Australia.

Image courtesy of Marco Capelli, RMIT University
U
nlike a regular biopsy where a patient’s tissue is harvested and sent to a lab for analysis, optical biopsies use ultra-thin endoscopes to look inside the body. This can be done either for diagnosis or during a surgical procedure and would normally produce a 2D image.
However, Dr Antony Orth and his colleagues at RMIT University have been using a light field imaging technique to produce microscopic 3D images in stereo vision, which could have revolutionary clinical applications. Stereo vision is the default format for human vision, where the eye takes in an object from two different viewpoints – namely, the left and right eyes – and uses this to process depth.
Orth, who has recently taken up a new position as a research officer at the National Research Council Canada (NRC) says: “Our 3D imaging technology works by looking at how light travels in optical fibres. If you want to reconstruct the 3D structure of an object, one way to do it is to measure the angles of the light rays that form the image of the object. What we did was to show that you can measure these angles using an existing technology - optical fibre bundles.”
Optical fibres are commonly used to carry light inside electric cables, which can boost the bandwidth of a broadband connection and be used to establish a high-speed internet connection or long-distance telecommunication system.
However, they can also be used for illumination and imaging by being wrapped in tight bundles which can carry light into, or images out of, confined spaces – such as the cavities of the human body.
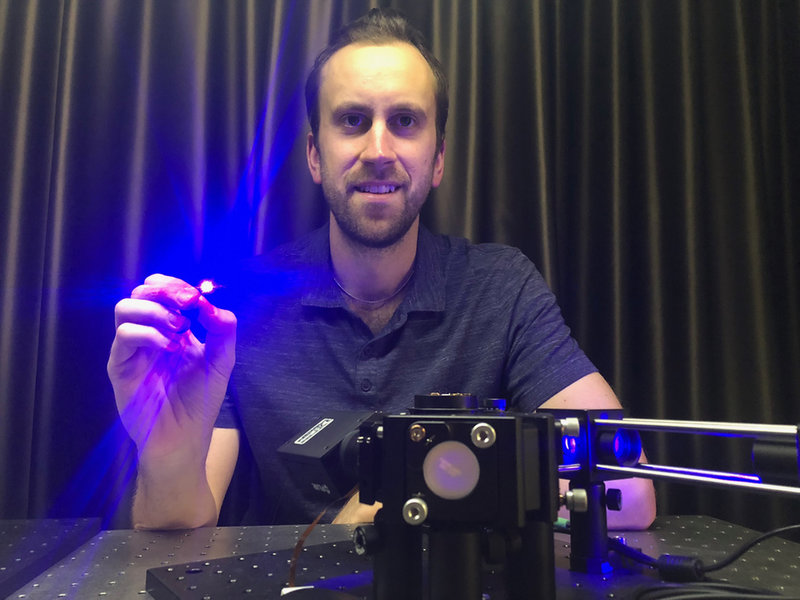
Dr Antony Orth. Image courtesy of RMIT University
The challenge of unscrambling information
The challenge here for clinicians is to unscramble the information they extract from the light field generated during an optical biopsy procedure and use it to produce a comprehensible image which will aid them in patient care.
Orth says: “When light enters the optical fibre bundle at an oblique angle, it tends to exit looking like a ring. On the other hand, when it enters the fibre bundle head-on, it tends to exit looking like a spot. By using this difference, we can quantify the angular distribution of light that entered the fibre bundle, and consequently the 3D structure of the object that is at one end of the fibre.”
The hypothesis is that an optical biopsy is more informative when the underlying data is 3D.
This approach borrows principles from the process of light field imaging, where multiple cameras look at the same scene from slightly different perspectives to create a ‘multi-viewpoint image’. By measuring the angles at which rays of light shone within the body bounce off of biological structures and back into the system, a clinician could work out the 3D structure of a microscopic fluorescent sample using just the information in a single image.
Orth says: “In a clinical setting, this may allow the clinician to assess the depth of a population of cells, or the topography of a microscopic part of the gastrointestinal tract. The hypothesis is that an optical biopsy - where the tissue is imaged for diagnosis without harvesting - is more informative when the underlying data is 3D instead of 2D.”
Understanding the medical value
The technology has yet to be used on any human subjects, it has only been trialled in a lab on biological specimens. Due to the fact that the technology uses the hardware of optical fibre bundles, which are already in common use, Orth and his team expect regulatory approval to be forthcoming.
The technology could be used for in vivo 3D fluorescence microscopy in biological research.
While the fundamentals of the technology have already been proved safe, the next steps are working out what the best clinical applications for the technology. It’s thought that as well as during optical biopsies the technology could be used for in vivo 3D fluorescence microscopy in biological research.
Orth says: “The next step is to apply this technology to a set of specific clinical questions to understand where the medical value lies. The technology itself is software based, so it is essentially ready for use already. The main challenge now is understanding how and where to use it from a clinical perspective.”